Hysteroscopy
A technique that is able to diagnose pathologies and perform intrauterine surgical procedures
A hysteroscopy is a simple and routine gynaecological examination technique that allows the interior of the uterine cavity to be examined.
In general, it is recommended when other examinations, such as gynaecological ultrasound, cytology or endometrial biopsy, indicate the existence of a possible intrauterine pathology.
Its application detects the presence of fibroids, myomas, polyps, uterine malformations or other problems, such as an exaggerated growth of the uterus, which can cause you to have heavy periods or bleeding outside the menstrual period.
One of its advantages is that the diagnostic examination can be done during the consultation and lasts no more than 2 or 3 minutes.

How is it done
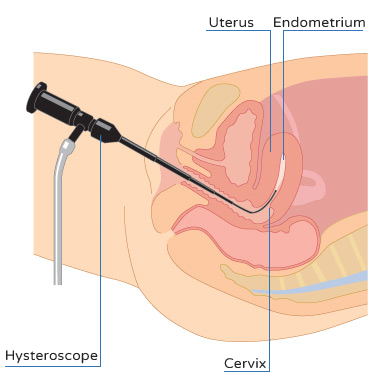
To do this, an endoscopic technique is performed, which consists of introducing a kind of flexible tube through the vagina and cervix. This probe is connected to a video camera and can inspect the shape of the inside of the uterus and endometrium.
To promote visibility, the hysteroscope - the name given to the instrument used for this examination - simultaneously administers physiological serum, which helps to expand the cavity, clear intrauterine mucus and provide a clear image for diagnosis.
Another advantage of this technique is that it allows a sample of cells from the endometrial mucosa to be taken for analysis (the study is called a biopsy).
In addition, the video camera allows you to comment on the examination and inform the patient while viewing the intrauterine images through a television monitor.
Who is it for
A hysteroscopy is indicated in patients who have been diagnosed with some type of pathology that can be observed using this technique, such as:
- Endometrial polyps.
- Submucosal fibroids.
- Uterine malformations such as septa.
- Inflammation.
- Adhesions after curettage.
- Some tumours.
Are there any contraindications?
Generally speaking, this examination can be performed on virtually all women, even those who have not had sexual intercourse, as the position of a speculum or vaginal separator is not necessary.
Sometimes, it may be necessary to take an anti-inflammatory before performing the examination, for example if you have painful periods or if you have a medical history that advises preventive consumption.
This examination may not take place in cases in which the cervix is very closed (naturally or due to previous surgeries), since this can obstruct the path towards the interior of the uterus.
Can there be any complications?
Like any medical procedure, this technique is not without its complications.
Therefore, before the test, the patient will be informed thereof via the appropriate informed consent form, but in our experience complications are rare.
How are pathologies observed by hysteroscopy?
This depends on the previous diagnosis.
- In the case of inflammation of the endometrium, which can cause pain in the lower abdomen or reproductive problems, such as miscarriages or implantation failures during in vitro fertilisation cycles, specific antibiotics, and sometimes also anti-inflammatory drugs are recommended.
- In the case of pathologies such as polyps, fibroids, adhesions or septa, the solution will be hysteroscopic surgery itself, as hysteroscopes that can perform manoeuvres with scalpels have been developed.
Is the surgery performed in the operating room?
It is not always necessary to perform hysteroscopic surgery in an operating room.
There are hysteroscopes that allow small procedures to be carried out in the practice itself, thus avoiding going to the operating room.
In any case, the procedure usually lasts no more than 5 minutes and in these cases you will always be accompanied by our nursing team who will assist you during the process.
When is surgery performed in the operating room?
It is performed in an operating room:
- As long as the woman wants it to be.
- When the hysteroscopist estimates that the procedure will take more than 5 minutes, which is a reasonable time to practice in consultation without anaesthesia.
- When the pathology to be treated is larger than normal.
- When more extensive procedures are to be performed, such as for a large myoma or an endometrial ablation, also known as an endometrectomy *
* Endometrectomy or endometrial ablation is a hysteroscopic technique that consists of trimming the entire layer responsible for menstruation in women who do not wish to have more children and who suffer heavy menstruations which do not allow them to go about their daily lives and cause phases of anaemia.
Return to normal life
The process of returning to daily activity after a hysteroscopy will depend case to case:
- For a diagnostic hysteroscopy consultation, which was recommended only to examine the interior of the uterus, it is not necessary to take any precautionary measure or special care. But if you're trying to get pregnant, you should avoid having sex until after your next period.
- For a hysteroscopic surgery consultation, it will depend primarily on whether you have taken relaxants, as they leave a feeling of drowsiness which will make you need to rest for the rest of that day. But from the day after, you'll be able to live an absolutely normal life in every respect.
- For hysteroscopic surgery in an operating room, somewhat more extensive procedures are performed under anaesthesia, so it is advisable to rest for a few days to control the discomfort. You should also avoid sexual intercourse and immersion in water (swimming pool, bathtub etc.). After that, you'll be able to live a normal life.
Our experience
At Dexeus Mujer we perform:
- Around 2,500 to 3,000 diagnostic consultation hysteroscopies each year.
- Approximately 250 consultative hysteroscopic surgeries per year.
- About 500 hysteroscopic surgeries in the operating room per year for the removal of endometrial polyps, submucosal fibroids, intrauterine adhesions, removal of malformations and endometrectomy ablations to control heavy menstruation.
Why choose us
The latest technology in diagnostic imaging and a team of radiologists specialising in the pathology diagnosis.
A team of surgeons who perform more than 1,500 gynaecological surgeries every year.
A committee of experts that meets weekly to individually evaluate each case and establish the guidelines you should follow.
Our own medical protocols allow us to react quickly should we detect any pathology.
Our facilities allow us to offer you all the security you need, as well as employing integrated circuit technology to centralise all diagnoses, treatments, consultations and interventions.
You will be in the best hands and in a first class hospital environment, with a 24-hour emergency service.
Testimony
Ana, 49 years old. Premià de Mar
"During a gynaecological check-up, a myoma was detected. At first I was scared, but the gynaecologist told me not to worry, although I did need to have a hysteroscopy to confirm the diagnosis and better observe it. The test was a little daunting, but it was actually very simple and I barely knew it was happening. The doctor performed the procedure during consultation and explained that in principle it was not necessary to operate, because it was very small, but to make a follow-up to observe how it evolves, because if they grow or change, then surgery can be recommended."



